Special delivery
With vector-borne disease evolving, climate gets a closer look
Sep 6, 2011 - by Staff
Sep 6, 2011 - by Staff
Bob Henson | 8 September 2011 • When Kristie Ebi talks about climate and health, she likes to show a photo she took of a newspaper ad posted by the Delhi health department that warns of the risk of mosquito-borne dengue fever. The sign exhorts residents to cover open containers of water around their households and lays out the consequences for not doing so: “17,665 persons have already been prosecuted in Delhi for causing mosquitogenic conditions and 32,020 legal notices have been issued.”
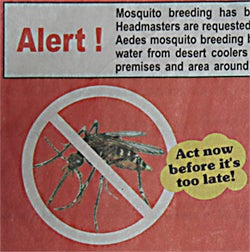
Part of a poster exhorting residents of Delhi, India, to do their part to reduce the spread of mosquito-borne dengue fever. (Image courtesy Kristie Ebi.)
If a basic step in disease prevention takes this much muscle, imagine the effort required to keep tabs on the global evolution of health threats in a changing climate. Ebi, an epidemiologist who now directs the technical support unit for Working Group 2 of the Intergovernmental Panel on Climate Change (IPCC), has been at this interface for 15 years. She’s among a small but active group of discipline-crossing specialists who are analyzing the response of disease transmission to temperature, moisture, and other atmospheric variables.
NCAR has formed its own nucleus of climate/health researchers over the last few years, with a varied set of projects that combine fieldwork and computer modeling. Teams from NCAR have assessed plague risk in Uganda, bacterial meningitis in Ghana, and the spread of dengue-transmitting mosquitoes in Mexico. And two postdoctoral researchers are now dividing their time between NCAR and the U.S. Centers for Disease Control and Prevention, or CDC (see box below).
A biannual colloquium at NCAR is one of the few places where a critical mass of climate and health researchers gather. The fourth such meeting, which took place on 11–15 July, drew more than 40 early-career and veteran scientists from a variety of disciplines, including climate modeling, statistics, epidemiology, and public health. More than a dozen state and local health experts were also on hand at this year’s meeting.
Among the main principles of the colloquium is that collaboration is not just helpful but essential. Ebi cautioned those embarking on research in climate and health: “Don’t try this by yourself. . . . You really need to build networks.” She organized the 2011 colloquium with NCAR’s Mary Hayden, a medical anthropologist; NCAR climate scientist Linda Mearns; George Luber, associate director for global climate change at CDC’s National Center for Environmental Health; Ben Beard, who coordinates CDC’s national programs on Lyme disease, plague, and tularemia; and CDC behavioral scientist Emily Zielinski-Gutierrez.
This year’s colloquium focused on vector-borne diseases, those transmitted to humans by fleas, mosquitoes, and other airborne go-betweens. Vectors, the pathogens they carry, and the hosts they infect are all influenced in one way or another by environment. The challenge for this group of scientists has been to decipher which aspects of disease spread are related to weather and climate and which are driven by other variables, which can include anything from public health initiatives to demographic trends and housing styles.

Malaria and climate is a keen interest of Madeleine Thomson (International Research Institute for Climate and Society), who spoke at the 2011 NCAR colloquium on climate and health.
“Disease transmission is multifactoral and multiscale, and climate is one of many factors,” notes Hayden. Even when the atmosphere isn’t the main driver, she adds, a small climate-related shift can have major implications when large numbers of people are involved.
Malaria is the world’s greatest infectious disease threat, with more than two billion people living in malarial regions, some 300 million infected each year, and almost a million deaths. In the highlands of western Kenya, reports of malaria increased alarmingly in the 1980s and 1990s—an observation that some attributed, at least in part, to global warming. A warming climate would be consistent with a more rapid development cycle for both the Anopheles mosquito, which transmits the parasites that cause malaria, and the parasites themselves. In theory, this could increase transmission in the traditionally cool highland areas.
But are warming temperatures actually to blame, or could other factors, such as drug resistance, be the main cause? Both climate and health experts had long been concerned about warming, but in a 2002 Nature paper, a leading team of malaria researchers headed by zoologist Simon Hay (University of Oxford) reported no evidence of warming in the Kericho Tea Estates, a tea-growing region located in the Kenyan highlands. With both meteorological and epidemiological data limited in the region, a pitched battle unfolded in science journals.
“The spat paralyzed the discussion of climate and health at the highest policy level,” wrote Madeleine Thomson (International Research Institute for Climate and Society, or IRI) and colleagues in a 2011 Nature overview.

Some of the biggest vector-borne threats for Americans in recent years have spread in ways that aren’t obviously related to climate. The most common vector-borne U.S. ailment is now Lyme disease, which struck at least 30,000 Americans in 2009.
The greatest incidence of Lyme disease, which is transmitted to humans by deer ticks, is in two distinct corridors: one along the heavily populated mid-Atlantic coast and the other stretching from eastern Minnesota to southern Wisconsin (see CDC graphic above).
In his colloquium talk, CDC’s Paul Mead speculated that Lyme’s recent emergence may be in part due to patterns of land use and deer population. He noted that Connecticut’s deer population, after being reduced through hunting to only a handful a century ago, has soared to around 100,000 today.
This isn’t to say that climate is irrelevant. Mead and colleagues examined the relationship between short-term meteorological variables and the seasonal onset of human Lyme disease in 11 states. About 60% of the year-to-year variability in Lyme transmission onset for a given state can be explained by a simple model based on growing degree days (a cumulative index of warm weather), relative humidity, and latitude, said Mead.
But the clustering of Lyme in some parts of the nation, and its virtual absence from regions like the U.S. South, remain a mystery.
Researchers can breach these hurdles through effective collaboration with the national meteorological agencies. “Real partnerships with key individuals are critical,” says Thomson. For example, when IRI’s Judy Omumbo teamed up with Kenyan meteorologist Sam Waweru, the institute was able to help analyze a 30-year set of daily temperatures for Kericho, where peak seasonal malaria rates had increased sevenfold since the 1980s. The results, published this year in Malaria Journal, confirmed that Kericho’s temperatures rose by roughly 0.2°C per decade between 1979 and 2009.
This doesn’t prove a link to malaria, notes Thomson, but it does keep open the possibility that warming temperatures could have played a role. Malaria rates across the Kenyan highlands have declined over the last few years. This suggests to Thomson that control measures are having an effect, though she adds that research is needed to find out if recent drought in East Africa is also playing a role: “When a disease is climate-sensitive, the climate should always be factored in as a possible contributor to change.”
In southern Mexico, a team of scientists from NCAR, NASA, Colorado State University, and the University of Veracruz is studying a different link between climate, health, and elevation. Through a multiyear NSF grant, they’re examining whether the city-dwelling mosquito that transmits dengue fever—Aedes aegypti—might move from the coastal region near Veracruz and expand its range westward and upward toward Mexico City, where it would threaten tens of millions of people. Already, dengue is one of the most widespread and fastest-growing infectious diseases on Earth, with as many as 100 million infections per year.
In order to track mosquito prevalence, the team is recruiting 50 households in each of 12 neighborhoods, most of them in urban areas along the study’s east-west corridor. Hayden and colleagues will hunt for mosquitoes—collecting them for later analysis—and evaluate the home environments, looking for ripped screens, open water containers, and other risk factors. The team’s first fieldwork took place this summer; they’ll continue to check each neighborhood periodically for mosquito presence and abundance into 2013.
Meanwhile, NCAR’s Andrew Monaghan will be leading an effort to model southern Mexico’s climate, and its suitability for Aedes aegypti, at high resolution. Along with conventional data sources, he’ll draw on about 20 weather stations that will gauge temperature and humidity at locations close to the mosquito sampling sites. “We’ve had to be very opportunistic about this,” says Monaghan of the instrumentation effort. A few of the sensors will be placed in schoolyards, with others going into the backyards of friends and family of the Veracruz scientists.
With these and other data, Monaghan and colleagues will simulate present climate and project it into the coming decades. To estimate the future trajectory of Aedes aegypti, they will combine the climate simulations with anticipated development patterns across the fast-growing region. Monaghan expects that the fate of Aedes aegypti will depend largely on whether the household living standards that serve as mosquito controls increase at the same pace as human population, with climate serving as a facilitator whose role he hopes to quantify.
Other mountainous tropical locations, such as Ecuador, may face similar situations as the climate warms, says Monaghan: “We’re hoping we can extrapolate our results beyond the Mexico transect.”
Although future changes in climate are a natural focus of interest when it comes to health, climate variability is a long-acknowledged player. One example came in the 1980s with the recognition of hantavirus disease and a rise in human plague cases across the southwestern United States. Neither was observed in great numbers—only a few dozen hantavirus cases and only a handful of plague diagnoses per year—but because both illnesses have high fatality rates, the increase was concerning.

During training sessions arranged by Ugandan health officials in September 2010, villagers learned the value of reporting plague cases via cell phones. Weather models are being explored as a tool for targeting prevention and reporting efforts. (Photo by Andrew Monaghan.)
Researchers soon related year-to-year trends in hantavirus to precipitation over the preceding winter. In the Southwest’s dry climate, generous winter rain and snow helps support the population of deer mice whose droppings and secretions spread the virus to humans. The story for plague is similar, as recounted at the NCAR symposium by CDC’s Ken Gage. Rats and other mammals carry plague and transmit it to humans, either through direct contact or through fleas that serve as vectors. As with hantavirus, the rodent hosts tend to be more populous after wet winters and springs.
Since the El Niño/Southern Oscillation largely dictates winter precipitation in the Southwest, public health experts found themselves with a useful predictive tool at hand. In a 2010 study, lead author Tamara Ben Ari (University of Oslo) found that plague transmission to humans was most likely when an El Niño coincides with the positive phase of the Pacific Decadal Oscillation.
In Uganda, the timing of rainfall appears critical to the risk of plague. Using a model with 2-kilometer (1.3-mile) resolution, NCAR’s Monaghan has produced a decade-long rainfall database for the mountainous area. Those data are now being correlated with plague reports. “The rainfall is episodic, and it’s spatially variable,” says Monaghan. The region sees about 200 cases of human plague each year, roughly 10% of the global total, and the study’s main funders—CDC and the U.S. Agency for International Development—are eager to keep those numbers low. “We hope to map hot spots for plague so that we can more effectively target intervention measures,” Monaghan notes.
Google.org has been investing heavily in climate and health research across Africa, including studies on disease outside the vector-borne realm. In Ghana, major outbreaks of bacterial meningitis tend to spike every few years during the dry season, though it’s not yet clear exactly why. NCAR is part of a team working with Google.org support to improve the production and dissemination of medium-range weather forecasts. By knowing when and where the rains will return, local health specialists can steer the flow of scarce vaccine to where it’s most needed. (See http://bit.ly/rhlwrD for more details and a slideshow.)
A running theme at this year’s meeting was how to synchronize health and climate data for maximum benefit. Climate modelers can tailor their output to serve the needs of health researchers, but only if they know ahead of time which meteorological variables are most important to track and save.
Tamara Greasby, who recently earned her doctorate in biostatistics, is working at NCAR with computational scientist Steve Sain on extracting data from the mammoth North American Regional Climate Change Assessment Program. The NARCCAP strategy involves six regional climate models that each draw on output from two of four global climate models, all looking into the next century using the IPCC’s A2 scenario.
“It’s great that we now have many more higher-resolution results from climate models, such as those from NARCCAP and a large number of global models,” says NCAR’s Linda Mearns, one of the colloquium’s organizers and the head of NARCCAP. “We can more thoroughly assess the uncertainty in future regional climate change, and by extension, the uncertainties in impacts such as those on human health.”
The climate of 2100 may not be known with rock-solid certainty, but it’s a safe bet that mosquitoes will adapt to it, pestering humans and spreading disease along the way. “This is an old group of insects,” noted Dan Strickman (U.S. Department of Agriculture) in his overview talk. “Mosquitoes have seen it all.”

Three of the current postdoctoral researchers at NCAR are basing their work at the intersection of climate and health. One of them, Katie Dickinson (center), is part of NCAR’s Advanced Study Program (ASP). The other two, Chris Uejio (right) and Sean Moore (left), are the first two participants in a unique two-year program, launched in 2010, that links atmospheric science at NCAR with health science from the U.S. Centers for Disease Control and Prevention.
Uejio is spending a year at NCAR, then moving to CDC’s National Center for Environmental Health in Atlanta this autumn for his second year. He’s extending research on water-borne disease and related meteorological factors that he pursued for his doctorate in environmental studies at the University of Wisconsin–Madison. Moore is staying in Colorado for the duration, splitting each week between NCAR’s Boulder labs and Fort Collins, where the CDC’s Division of Vector-Borne Diseases is located.
Moore is working with NCAR and CDC scientists to develop climate-based early-warning models for vector-borne infectious diseases, including Lyme disease (see box above), and studying the influence of interannual climate and weather variability on vectors and pathogens, with the goal of predicting when and where disease outbreaks are most likely.
Although Dickinson isn’t part of the NCAR/CDC program, its presence was a draw—“There’s a real community here”—and the flexible structure of ASP is allowing her to carry out similar research. Dickinson’s background includes a policy-focused undergraduate degree in Earth systems at Stanford University and a doctorate from Duke University in environmental economics. She’s now exploring several lines of work that include meningitis vulnerability in Ghana and hurricane risk in the United States. “The thing that interests me is behavior—why people do what they do, and how that affects their exposure to environmental and health risks.”